Weight Loss Tips for Inflammatory Arthritis
Mar 25, 2021Note: Reshape Physical Therapy and Wellness evolved into Weight Loss for Health, and finally Zivli. How to Lose Weight After 50 was our first course that eventually grew into Zivli. Some old blog posts or resources mentioned in this episode may have been removed.
Do you have inflammatory arthritis, pain, or limited mobility? If you want to lose weight, you may feel like you're at a huge disadvantage.
While exercise helps maintain your metabolic rate during weight loss, it's not essential to lose weight. Dr. Jason Fung wrote in The Obesity Code, “Exercise is like brushing your teeth. It’s good for you and should be done everyday, just don't expect to lose any weight.”
Exercise is one piece of the puzzle to lower insulin resistance. There are many other areas you can optimize first. Once you get some consistency and weight off, exercise will be easier.
Listen to This Episode
Highlights From This Episode
[0:00] Topic Intro
[3:15] What is insulin resistance?
[6:24] Insulin resistance quiz.
[7:22] The link between insulin resistance & osteoarthritis.
[9:45] Which medications may raise insulin resistance?
[13:02] Why to reduce added sugar to reduce inflammation.
[15:47] Why to increase protein with arthritis.
[19:38] Why to increase health fats to reduce inflammation.
[26:11] Why to use intermittent fasting to reduce inflammation.
What is Insulin Resistance?
Insulin is a hormone made in your pancreas. It serves many purposes in the body. It lowers your blood sugar and is the primary determinant of your body set weight.
Keeping blood sugar and insulin low reduces chronic inflammation. Reducing inflammation lowers your risk of type 2 diabetes, heart disease, dementia, cancer, arthritis, and more.
When you eat a meal, especially one high in carbohydrates, you’ll create a lot of blood glucose. That glucose moves from your blood into your cells.
The blood glucose can get into the cells in one of two ways. Muscle demand, or insulin.
Think of the glucose receptors on the cell as the lock. When insulin binds to its receptor, it acts like the key. Glucose can then move out of the bloodstream and into your cells.
The problem comes when you develop a resistance to your own insulin. This happens when insulin is too high for too long.
You may be familiar with other forms of resistance. For example a resistance to pain or sleep medications. Same scenario with insulin. You need more insulin to maintain the same level of blood sugar.
Insulin is your fat storing hormone. The higher your insulin levels, the higher your body set weight. The lower your insulin levels, the lower your body set weight.
When you start using, “How will this affect my insulin?” as your litmus test for if a choice is healthy, not “How many points or calories does this have?” you will see improved weight loss results.
Here’s where the good news comes for you if you have limited mobility and want to lose weight. Losing weight is about lowering your insulin! You may have thought you had two tools in your weight loss toolbox. Eat less, and exercise more. But there are so many things that impact your insulin levels!
Insulin Resistance Quiz
The book Why We Get Sick by Dr. Benjamin Bikman is helpful to understand insulin resistance. He makes a clear link between insulin resistance a many diseases.
This quiz is from his book. You can estimate your insulin resistance risk without bloodwork.
Mentally answer each of the following questions. If you answer yes to one of the questions, you likely have insulin resistance. If you answer yes to two or more of these questions, you most certainly have insulin resistance.
-
Do you have more fat around your belly than you’d like?
-
Do you have high blood pressure?
-
Do you have a family history of heart disease?
-
Do you have high levels of blood triglycerides?
-
Do you retain water easily?
-
Do you have patches of darker-colored skin or little bumps of skin (“skin tags”) at your neck, armpits, or other areas?
-
Do you have a family member with insulin resistance or type 2 diabetes?
-
Do you have polycystic ovarian syndrome (PCOS; for women) or erectile dysfunction (for men)?
Notice here that several of the questions asked for family history. If you DO have diabetes or heart disease, you absolutely have insulin resistance. If you have a family member that does, it's only a risk factor.
Osteoarthritis and Insulin Resistance: What’s the Link?
Here is a paraphrased excerpt from Why We Get Sick that explains the connection between insulin and osteoarthritis.
Osteoarthritis, or the loss of joint cartilage, is common in obesity. Because of the prevalence, many physicians thought obesity caused osteoarthritis. The classic “wear and tear” on the joints. Osteoarthritis is increasingly considered a metabolic disease.
Out of a broad range of overweight individuals researchers studied, those with osteoarthritis were most likely to have the highest insulin levels.Every cell in your body has an insulin receptor, even the cells in your joints. An essential component of the joint is the cartilage. Cartilage is the smooth, flexible connective tissue lining the ends of the bones.
The main cells in cartilage are chondrocytes and these are receptive to insulin. They are responsible for creating and maintaining the cartilage lining, or matrix. Chondrocytes need glucose to function.The chondrocytes need insulin to take in that glucose.
An insulin-resistant chondrocyte can’t maintain that matrix. As a result, the cartilage weakens. Another essential component of a joint is the “grease” for the joint—synovial fluid. Synovial fluid is made from cells called synoviocytes. When synoviocytes are exposed to high levels of insulin, they experience an invasion of immune cells.
These immune cells increase inflammation in the joint and reduce synovial fluid production.Without this grease, the joints grind. Osteoarthritis is not rheumatoid arthritis, or RA. RA is a chronic inflammatory joint disease. Because of the inflammation, RA increases the likelihood of developing insulin resistance.
How to Lower Insulin Resistance & Lose Weight Without Exercise
Tip #1: Check See if Your Arthritis Medications Are Contributing to Insulin Resistance
Many people with joint pain take medications to help reduce their pain. Some of these medications increase blood glucose. Increased blood glucose will increase insulin resistance. Your pain is better, but insulin resistance is worse.
Glucosamine in some form, which may improve joint health and reduce joint pain. But evidence for these supplements are ambiguous and open to debate.
While glucosamine may improve your joints, it does contribute to insulin resistance. It’s not the only medication that you could be impacting your weight. You may be taking more than one of these medications. This has a compounding effect on your metabolism.
Other common pain and swelling medications that raise insulin resistance include:
- Steroids such as hydrocortisone and prednisone
- COX-2 inhibitors like Celebrex (celecoxib)
Topical creams do not raise blood glucose and do not have an impact on insulin resistance.
If you feel like you do need medication for your pain, talk with your physician. Together you can determine the best course of action for you. If you already have diabetes, be aware how your medications affect your blood glucose.
Have a glucometer in your house and know how to use it.
Glucosamine, steroids, and celebrex may not help you lose weight. Consider pain relief options that won’t raise insulin.
If you’re not in a place where you feel you can change your medication regime, I have a few more helpful tips. These that will lower insulin resistance and inflammation. Best case scenario, you can reduce your need for pain medications. Then you'll lose more weight, and have more desire to exercise.
Tip #2: Reduce Added Sugars
Added sugar is a type of carbohydrate. there are three main macronutrients, carbohydrates (starch, sugar, fiber); proteins; and fats. Not all carbs, proteins, or fats impact insulin and inflammation the same.
Processed and refined sugars and starches spike blood sugar levels. This leads to a spike in insulin. Added sugar is a double whammy because it triggers the same reward center in the brain as cocaine. Sugar begets sugar, the more you have, the more you’ll want.
The human body has only about 4 grams, or one teaspoon of sugar in its 5 liters of blood. So when you flood it with added sugar, that’s a huge stress on your body. It tries to get rid of it as fast as possible to return to its 4 teaspoon baseline.
The American Heart Association recommends women have no more than 24 grams of added sugar per day, and men have no more than 36.
Added sugar, like table sugar, is 50% glucose and 50% fructose. Glucose can be used anywhere in the body. Starchy foods like bread and pasta are 100% glucose. But fructose is metabolized almost exclusively in the liver.
The liver has a limited capacity to metabolize fructose. If it gets too much at a time, it’s immediately turned into liver fat. A fatty liver is not an efficient liver.
Added sugar is hiding in so many processed foods. There are over 200 different names for added sugar.
I recommend you start looking at your food labels and zero in on added sugar. It’s going to be hard to avoid all together. Making a consistent effort to eat less refined sugar is one of the best things you can do for your health.
If you have a problem with sugar, watch Fed Up documentary. It's motivating to quit the habit. Google, “Watch the Fed Up Documentary” and several options will come up for you.
Tip #3: Prioritize Protein
Most of my clients are not eating enough protein when they start my program.
Protein is essential for healthy muscles. Healthy muscles are essential for healthy joints and bones. The 2020 U.S. dietary guidelines recommend adults get 5 ⅕ ounces of protein per day. 5 ½ ounces of chicken is about 45 grams of protein.
The new government guidelines are confusing and unfortunately not very helpful.
The research I’ve found suggests 1.1 - 1.5 grams of protein per kilogram of body weight per day. I aim for 2.2 grams per kilogram of ideal body weight...or to make the math simpler, 1 gram per pound of ideal body weight.
For example, if your ideal body weight is 140, aim for 140 grams of protein. This is the amount recommended to build muscle. As we age, we face the harsh reality of sarcopenia, or a natural loss of muscle mass. We all should focus on building muscle. If you’re not building, you’re losing.
Prioritizing protein has a couple more benefits for weight loss. First, it’s very satiating. Unlike refined carbs, protein and fats will trigger your satiety hormones. These help keep you fuller for longer.
Second, protein has a higher thermogenic effect of food. Your body has to use more energy to break down the protein you eat compared to carbs. Sugar cravings go down when you you eat more protein.
Adults should aim for at least 30 grams per meal. That’s the threshold needed for optimal muscle protein synthesis. Having 10 grams of protein at a meal won’t cut it. You need the proper total amount, dosed high enough, to build muscle.
There are a few distinct advantages to having more lean muscle mass. First, the more muscle you have, the higher your metabolism.
Second, in the average middle-aged person, muscle accounts for roughly 25%–30% of body mass. This means muscle is the largest insulin-sensitive tissue in the body.
When it comes to insulin resistance, muscle is very important! How much of it we have, and how insulin sensitive it is, is vital in determining how insulin sensitive we are.
This is because muscle can take up glucose from the blood. In response to insulin; as glucose drops, insulin returns to baseline. As the amount of muscle increases or decreases, insulin sensitivity changes accordingly.
If we have more muscle, we have more “room” to deposit glucose, which helps keep insulin low.
Tip #4: Increase Healthy Fats
Fats, while they are higher in calories, have the lowest insulin response of all three macronutrients.
Focus on increasing your consumptions of bioavailable omega-3 fatty acids. Reduce your consumption of processed omega-6 fatty acids and trans fats. Watch this video or download next. Our Ultimate Food Guide explains healthy, neutral, and unhealthy fats.
Both omega-3 and omega-6 fatty acids are essential, meaning the body can’t make them and you have to get them from food.
There are several different kinds of omega-3 fatty acids but the most common are EPA, DHA, and ALA.
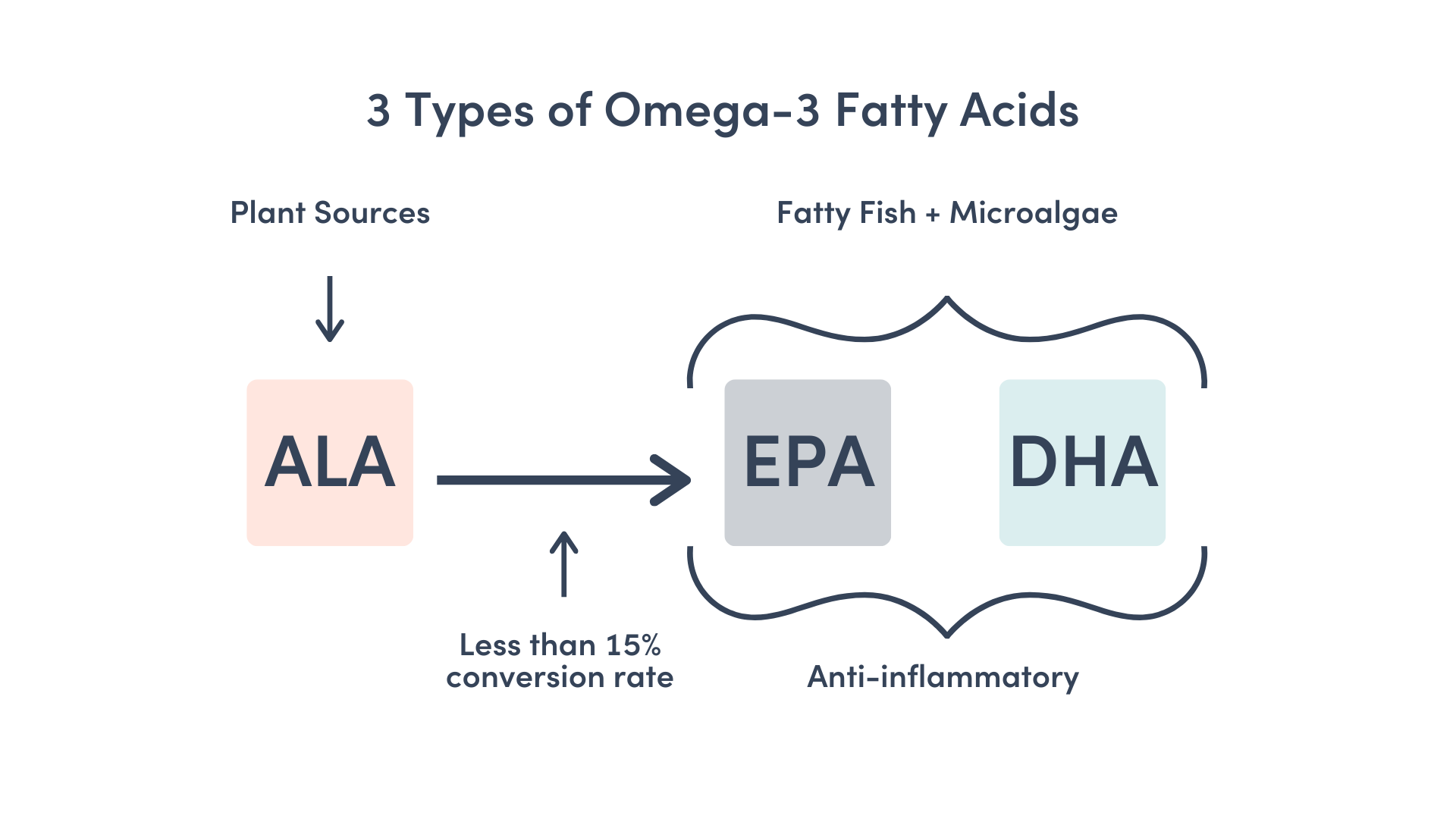
Most people are not eating enough fatty fish and green algae to get the recommended amount. They may be eating good plant sources that have high amounts ALA. But the conversation rate to EPA and DHA is pretty low, less than 15%.
That’s why many doctors and registered dietitians will recommend an omega-3 supplementation.
It’s good to aim for fatty fish a couple times per week in your diet. Examples include salmon, herring, mackerel, trout, sardines, tuna, and halibut.
Plant sources of omega-3 fatty acids include: flaxseeds, flaxseed oil, chia seeds, avocados, avocado oil, olives, cashews, walnuts, and almonds.
The recommended ratio of omega-6 to omega-3 fatty acids is 4:1 to 2:1. The standard American diet that is so high in processed and fried foods has a ratio closer to 10:1 to 50:1.
To reduce this ratio and lower your inflammation, reduce or seed and vegetable oils oils.
Linoleic acid is one type of omega-6. It is the most easily oxidized type of fat. This oxidation contributes to atherosclerosis, inflammation, and insulin resistance.
I recommend coconut oil, olive oil, avocado oil, butter, or ghee for cooking. Avoid canola oil, corn oil, soybean oil, and other oils. Avoid fried foods because they are usually fried in one of these types of processed oils.
Levels of linoleic acid are much lower and less harmful when found naturally in foods like many nuts.
Stress management, sleep, and movement are important to reduce insulin resistance as well. I didn’t leave them out for any other reason than to help you prioritize your efforts on nutrition.
With optimized nutrition, your metabolic, physical, and psychological stress levels will drop. You may experience improvement in sleep quality as well.
Tip #5: Intermittent Fasting
Intermittent fasting is one of, if not the most effective way to lower insulin resistance. When you fast, you’re giving your body the chance to rest and digest. Fasting is also a proven way to lower inflammation, help you tap into your fat for fuel, and get autophagy.
Autophagy is "self-eating." It’s the body's way of cleaning out damaged cells to regenerate newer, healthier cells.
Autophagy starts at about 16 hours of fasting. To get more of a benefit, you’ll want to work your way up to longer fasting periods if your goal is autophagy.
Remember that intermittent fasting is not about eating less, it’s about eating less often. You’re shifting your mindset from “How do I eat less calories” to “How do I lower insulin?”
You are fasting anytime you’re not eating. I encourage people to start with a 12 hour fast. This usually eliminates any late night snacking and immediately improves sleep quality. Then, aim for a daily 14 hour fast. This allows your insulin to drop back down to baseline.
I like the 5-1-1 schedule for fasting. Five days a week I’ll aim for a 14-16 hour fast, one day a week I fast for 24 hours, and one day a week is a flex day. I advocate for structured flexibility. No food is off limits, there are no last meals. There’s no point in living a restrictive lifestyle you can’t maintain.
In Why We Get Sick, Dr. Bikman reported that patients who fast for 24 hours roughly once monthly are about half as likely to be insulin resistant compared with those who don’t.
Subscribe & Review
Subscribing and leaving a rating and review are important factors in helping the Reshape Your Health Podcast and the YouTube Channel reach more people. If you haven't already subscribed, please do that today.
We would also be grateful if you left a rating and review, too. In your listening app, scroll to the “Ratings and Reviews” section, then click “Write a Review” and let us know what you enjoy about our show. We appreciate you taking the time to show your support. Thank you!
Resources From This Episode
>> Join Zivli
>> Freebie: Weight Loss Mindset Audio Training
>> Freebie: The Ultimate Food Guide
>> 5 Foods That Raise Inflammation Episode
>> 5 Foods That Lower Inflammation Episode
>> Why We Get Sick by Dr. Benjamin Bikman
>> The Obesity Code by Dr. Jason Fung

